Name and role of Lead
Tim CH Hoogenboom, Head of Research, Open Medical
About Pathpoint ePOA
Pathpoint ePOA is a digital innovation designed to enhance preoperative assessment (POA) services within the NHS, a crucial part of elective care pathways. In the UK, POA ensures patients are assessed for medical fitness and suitability before planned surgery. This assessment can be conducted through various modalities, including in-person consultations or remote digital interactions. It is typically led by specialist POA nursing staff within dedicated POA clinics at an NHS Trust, with anaesthetic input when required. POA services are fundamental to effective perioperative care, aiming to ensure patient safety, surgical readiness, and optimal clinical outcomes while contributing to efficient resource utilisation.
Pathpoint ePOA is a module within Open Medical's broader Pathpoint Surgicare platform, designed to support more sustainable surgical pathways. This case study focuses on the ePOA module, the challenges it addresses, and the estimated carbon and financial impacts achieved through its implementation.
The Challenge
POA is a critical component of the surgical pathway, ensuring patients’ health are optimised and care plans are tailored. Delivering timely and effective POA is essential to allow for necessary health optimisation, without assessments becoming outdated and requiring duplication of effort and resources. A POA assessment typically remains clinically valid if conducted within three months of planned surgery.
However, increasing demand for elective care, growing patient complexity, and NHS workforce pressures contribute to POA backlogs. This leads to assessments occurring outside the optimal timeframe, either too early, risking duplication of tests and appointments, or too close to surgery, increasing the risk of last-minute cancellations. These disruptions affect patient experience, operational efficiency, and care quality.
Both scenarios generate significant environmental impacts and inefficiencies. Unnecessary appointments and repeat assessments result in avoidable patient travel, increased use of resources, and higher energy consumption. These factors increase NHS Carbon Footprint and financial costs, ultimately diverting resources from frontline care.
Pathpoint ePOA addresses these challenges by digitising and streamlining the POA pathway. It facilitates earlier identification of patients for prehabilitation and supports a more sustainable model of care. This approach improves care quality and efficiency, reduces waste and lowers emissions, contributing to a Greener NHS.
Innovation
Pathpoint ePOA is a cloud-based digital health platform designed to digitise POA workflows within elective surgical pathways. It enables clinical teams to efficiently assess a patient’s fitness for surgery, identify individuals for prehabilitation, and coordinate care through an integrated, collaborative platform.
Supported by the SBRI Healthcare, Open Medical improved their existing Pathpoint ePOA, operational at West Hertfordshire (WHH) Teaching Hospitals NHS Trust by integrating a complexity stratification algorithm. This upgrade enables the system to attribute a ‘complexity score’ for every patient, facilitating the POA team to quickly identify patients with complex comorbidities. Patients assessed as low or medium complexity can follow more resource-efficient, lower-carbon care pathways.
When a patient is listed for surgery, a digital POA pathway is triggered in Pathpoint. Patients receive an automated notification via SMS or email with a link to complete a digital health questionnaire remotely, eliminating travel need. Pathpoint ePOA analyses the responses and generates a complexity score (low, medium, or high). This guides the clinical team in arranging appropriate follow-up. This approach aligns with Get It Right First Time (GIRFT) principles for early screening of patients.
Pathpoint ePOA is currently live in three NHS Trusts. It is available through established procurement frameworks including G-Cloud, LPP CDH, or direct SLA. The solution is offered on a subscription basis with a 30-day exit clause, allowing for low-risk trial and adoption. This commercial model offers a scalable, cost-effective and adaptable route to digital transformation.
More information: https://www.openmedical.co.uk/epoa
Impact
Methodology:
Current and previous Pathpoint ePOA models were compared to assess whether the current model introduces carbon and financial savings. The current model includes a complexity stratification and extends POA validity from three to six months for ASA I and II patients.
Using data from 01/06/2024 to 04/05/2025, the distribution of patient complexity and number of repeat POAs in both models were determined. Resource requirements and changes to nursing involvement were used to estimate associated carbon emissions and financial costs.
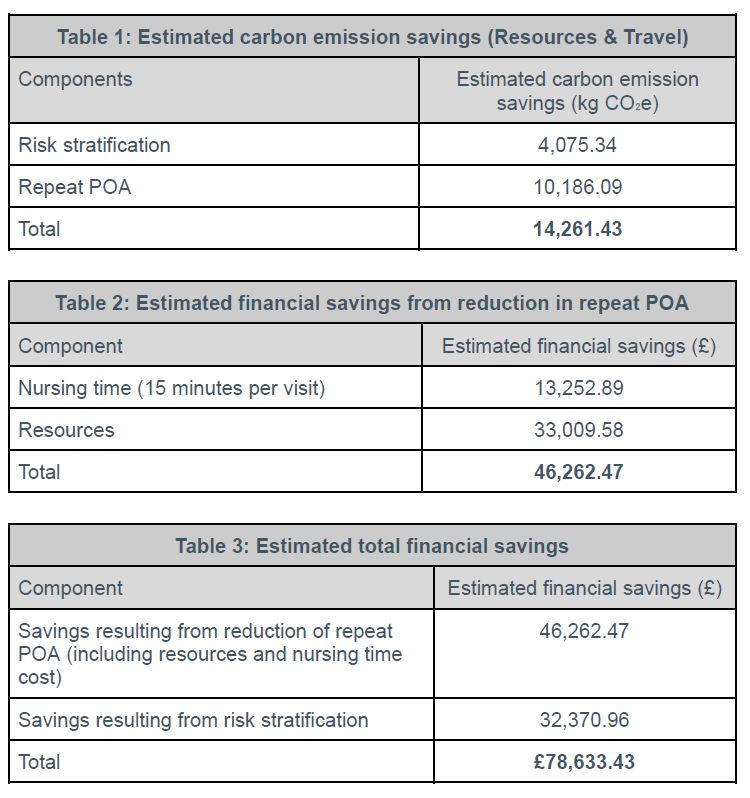
Carbon savings (Table 1):
Patients previously managed as medium-complexity can now be assessed as less carbon-intensive low-complexity, resulting in an estimated carbon saving of 4,075.34 kg CO₂e. In addition, extending POA validity reduced the number of repeat assessments, avoiding an estimated 1,561 additional in-person visits. This led to a further carbon saving of 10,186.09 kg CO₂e.
These changes in the current Pathpoint ePOA model delivered a total estimated carbon saving of 14,261.43 kg CO₂e, equivalent to driving approximately 67,526 miles (108,673 km) in an average petrol car[1].
Financial savings (Table 2 and 3):
The reduction in repeat assessments also saved approximately £46,262.47, when considering 15 minutes of nursing time per visit[2], and a repeat full blood count and ECG for expired POA.
The complexity stratification enabled patients to be assessed as “low complexity”, requiring fewer clinical resources. This contributed an additional saving of £32,370.96. Combined, the use of extended POA validity and complexity stratification generated an estimated total financial saving of £78,633.43.
References
-
Yurday E. Average CO2 Emissions per Car in the UK [Internet]. NimbleFins. 2020. Available from:
https://www.nimblefins.co.uk/average-co2-emissions-car-uk -
National Institute for Health and Care Excellence Preoperative tests (update) Routine preoperative tests for elective surgery NICE guideline NG45 [Internet]. Available from:
https://www.nice.org.uk/guidance/ng45/evidence/appendix-m-economic-considerations-for-delphi-pdf-87258149464
Next Steps
Further development and evidence generation:
Open Medical are continuing collaborative development with West Hertfordshire (WHH) Teaching Hospitals NHS Trust to refine how the complexity stratification algorithm can further optimise POA processes. The goal is to safely increase the proportion of patients managed through lower-carbon, lower-resource pathways. For example, adjustments such as raising the alcohol threshold for low-complexity classification are under review. The team are also seeking funding to support a comprehensive assessment of ePOA’s impact on surgical outcomes, including length of stay and complication rates, which influence both carbon and financial cost.
Implementation and evaluation:
The improved ePOA model, aligned with GIRFT principles, will serve as the blueprint for wider adoption across other NHS Trusts. Furthermore, sustainability metrics are now embedded in the internal evaluation framework, ensuring future deployments benefit patients, clinicians, and the environment.
Regulatory and international expansion:
Pathpoint ePOA meets current NHS regulatory and governance standards. The team are working towards CE marking to support international deployment. Outside the UK, Open Medical is already active in the Republic of Ireland and the Kingdom of Saudi Arabia where Open Medical recently completed a pilot project incorporating key learnings from ePOA, demonstrating the platform’s adaptability to varied clinical contexts and local challenges. Expansion across EU markets is also being pursued.

Date published
June 2025

