Innovation
Whole-body MRI (WB-MRI) screening for early cancer diagnosis in Li Fraumeni syndrome
Competition
NHS Cancer Programme – Innovation Open Call – Competition 2

Name & role of Project Lead
Dr Angela George, Principal investigator, Clinical Director of Genomics and Consultant Medical Oncologist in Gynaecology, The Royal Marsden Hospital
Clinical Problem
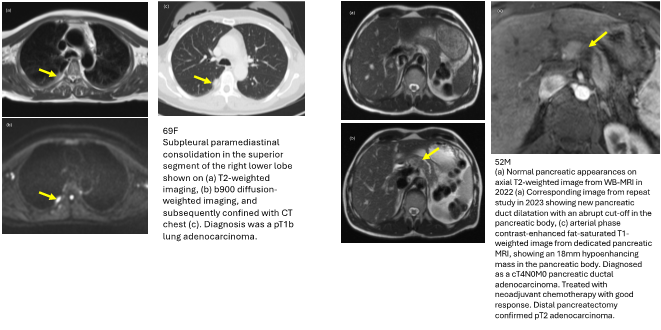
Li Fraumeni syndrome (LFS) is an inherited familial predisposition to a wide range of cancers. This is due to an alteration in the tumour suppressor gene TP53. LFS individuals have a 70-90% lifetime risk of developing cancer, often before the age of 50. The only screening for TP53 mutations in the NHS is annual MRI breast for females, therefore all the other cancers are not routinely screened for. A whole-body MRI (WB-MRI) scan looks at the body from head to toe to find cancers, aiming to detect tumours when these are very early and potentially curable.
Proposed Solution
The solution proposes that patients with LFS undergo annual whole-body magnetic resonance imaging with diffusion weighting (WB-MRI with DWI) in addition to usual care (e.g. Breast MRI and symptom awareness). WB-MRI with DWI is a recent but standard technology within the NHS used more commonly for imaging of multiple myeloma, melanoma and prostate cancer. It is not in routine clinical use in the NHS for inherited cancer syndromes. An implementation pilot as a service evaluation has been undertaken at the Royal Marsden Hospital and 50 patients with LFS have been enrolled in the study. The aim was to demonstrate that WB-MRI is a cost-effective tool in detecting early tumour and can be established as standard of care of screening in adults with LFS.

Market Traction & Implementation
• This project was completed at the Royal Marsden Hospital, a leading cancer hospital in the UK and Europe.
• The project has demonstrated that WB-MRI could detect early cancers in asymptomatic patients with Li Fraumeni syndrome.
• In the cohort, ten cancers were diagnosed with the help of WB-MRI. Seven cancers (70%) were early stages (TNM stage 0-2) and were treated with curative intent; three cancers (30%) were late stages (TNM stage 3-4).

Impact - Early detection & diagnosis of cancer
The project has demonstrated that WB-MRI is a valuable and useful radiological tool for detecting early cancers in patients with LFS and should be implemented as a regular screening test for this population. A health economics analysis is ongoing to determine if screening with WB-MRI is cost-efficient.
Clinician Quote
"Whole-body MRI in Li Fraumeni patients has the potential of diagnosing cancers when they are very early, when treatment with a curative aim is still possible. By offering a WB-MRI to this population, which is at very high risk of developing cancers throughout their lifetime, we can improve early detection, offer effective treatments and ultimately a better outcome and quality of life. " - Dr E Finn, Clinical Research Fellow, Study Physician
"Li Fraumeni, or more so, cancer, has dominated my family's lives for many years, from growing up not ever knowing my grandmother to losing my sister at the age of 34. I know for a fact that if we had had these MRIs our family history would be so different, and my hope is that with these on offer my family's future will be better. It has, in my opinion, already saved my life this year."
LG, Li Fraumeni patient
Date Published
February 2025

